Flashes & floaters
Spots or floaters are small, semi-transparent or cloudy particles within the vitreous, (which is the clear, jelly-like fluid that fills the inside of your eyes). They are quite common especially as you get older and usually, but not always, harmless.
Appearing as specks, threadlike strands or cobwebs, floaters are most visible when you look at a light background, such as the sky or a white surface. Spots and floaters are caused by:-
- Deterioration of the vitreous fluid, which is part of the natural ageing process.
- Certain eye diseases or injuries.
- Small flecks of protein or other matter trapped during the formation of the eye before birth.
Seeing flashes or streaks of light usually mean that the vitreous is shrinking. It may become detached from the back of your eye. Vitreous detachment is common and rarely leads to serious eye problems. However, it is very important that these flashes are checked immediately as they may also be a symptom of retinal detachment, which although rare, requires urgent hospital treatment.
Although spots and floaters are usually harmless, you should see your optometrist for a thorough eye examination when you first begin to see them or when you notice changes or increases in them. The optometrist can determine if what you are seeing is harmless or if they are the sign of an eye health problem in need of treatment.
Posterior Vitreous Detachment (PVD)
What is Posterior Vitreous Detachment?
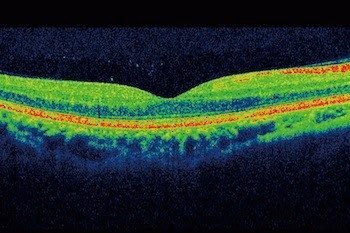
With age, the vitreous becomes more fluid and less jelly-like. As the eyeball moves, small pockets of liquid vitreous can move around inside the vitreous cavity. This movement causes the vitreous to pull on the retina, and, with time, the vitreous can separate from the retina. This is called posterior vitreous detachment (PVD) because it usually happens at the back (posterior) of the eye. PVD happens in most people eventually and rarely causes an eye problem.
PVD occurs in about 75% of people over the age of 65.
What is the vitreous?
The vitreous is a clear jelly-like substance within the eye that takes up space behind the lens and in front of the retina (the light-sensitive layer at the back of the eye). It is 99% water. The other 1% consists of substances which are important in maintaining the shape of the vitreous. The outer part of the vitreous (the cortex) has the highest concentration of collagen. The vitreous is attached to the retina, more strongly in some places than others. When a PVD starts the jelly pulls away from the retina.
Why does the vitreous detach?
The firm jelly-like substance of the vitreous changes with age. The central part of the vitreous becomes more liquid and the outer part (cortex) peels away from the retina. As it comes away from the retina it can cause the symptoms of posterior vitreous detachment (PVD).
What are the symptoms of PVD?
Many people are not aware that they have developed PVD but some notice symptoms such as floaters or flashing lights. Floaters can take many forms from little dots, circles, lines, to clouds or cobwebs. Sometimes people experience one large floater, which can be distracting and make things difficult to read.
The flashing lights that occur are also caused by the PVD. As the outer part of the vitreous detaches from the retina it can pull on this light-sensitive membrane, especially where the vitreous is attached quite strongly to the retina. The pull of the vitreous in these areas stimulates the retina. This stimulation causes the sensation of flashing lights since the brain interprets all stimulation signals from the retina as light.
Can anything be done to help with the PVD?
Unfortunately at the moment, nothing can be done medically for this condition, usually, people find that the symptoms calm down after about six months and people do eventually get used to living with the floaters. The brain tends to adapt to the floaters and eventually is able to ignore them, so they then only become a problem in very bright light.
Will I lose any sight?
Posterior vitreous detachment does not in itself cause any permanent loss of vision. Your visual acuity should remain the same, that is, you will be able to see just as you could before the PVD tarted. You may have some difficulties, to begin with, because of the floaters and flashing lights though these do not cause permanent sight loss.
The only threat to vision is the small chance of a retinal tear leading to a retinal detachment.
It is important to stress that retinal tears and detachments are much rarer conditions and that very few people with PVD go on to develop either of these problems. However, if you are concerned or uncertain ask your optometrist to check your eyes.
Retinal Tear and Vitreous Haemorrhage
Where the vitreous is securely attached to the retina, posterior vitreous detachment may cause the retina to tear. If the retina tears across a blood vessel, there will be bleeding into the vitreous – this is called vitreous haemorrhage. Small amounts of bleeding cloud the vision, leading to the sensation of walking through a swarm of insects – more severe bleeding leads to a mass of red or black lines, and vision may become very dark. A retinal tear is a serious problem; vitreous haemorrhage is even more serious and needs to examined promptly by an eye specialist.
Retinal tears may be sealed with a laser or cryotherapy (freezing), or both, to prevent retinal detachment. Both these treatments seal the retina to the wall of the eye, repairing the tear and preventing detachment.
Retinal detachment
What is the retina?
Imagine that your eye is like a camera, and the retina is the film. The retina is a fine sheet of nerve tissue lining the inside of the eye. Rays of light enter the eye and are focused on the retina by the lens. The retina produces a picture that is sent along the optic nerve for the brain to interpret. It’s rather like the film in the camera being developed so that pictures can be produced.

What is retinal detachment?
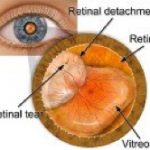 Usually, the retina is attached to the inner surface of the eye. If there is a tear or hole in the retina then fluid can get underneath it. This weakens the attachment so that the retina becomes detached – rather like wallpaper peeling off a damp wall. When this happens the retina cannot compose a clear picture from the incoming rays and your vision becomes blurred and dim.
Usually, the retina is attached to the inner surface of the eye. If there is a tear or hole in the retina then fluid can get underneath it. This weakens the attachment so that the retina becomes detached – rather like wallpaper peeling off a damp wall. When this happens the retina cannot compose a clear picture from the incoming rays and your vision becomes blurred and dim.
What is a vitrectomy?
If the retinal detachment is too severe for scleral buckling or pneumatic retinopexy (see below), surgery to reattach the retina may be necessary. Under general anaesthetic, the surgeon removes the vitreous entirely, replacing it with air or a fluid compatible with the eye. Over time, the fluid (or air) is absorbed, and replaced with the eye’s own fluid. Lack of vitreous does not affect the patient’s vision.
Who is more likely to get retinal detachment?
The detachment of the retina is more common in middle-aged, short-sighted people. It is quite an uncommon condition however and only about one person in ten thousand is affected.
Very rarely, younger people can have a weakness of the retina often associated with short-sight.
What are the symptoms?
The most common symptom is a shadow or veil spreading across the vision of one eye. You may also experience bright flashes of light and/or showers of dark floaters. These symptoms are never painful.
Many people experience flashes or floaters. These are not necessarily a cause for alarm, however, if they are severe and seem to be getting worse, and/or you are losing vision then you should see an optometrist or eye specialist urgently. Prompt treatment can often minimise the damage to your eye.
What is the treatment?
If you get help early, it may only be necessary to have laser or freezing (cryotherapy) treatment. This is usually performed under a local anaesthetic.
Often, however, an operation to repair the hole in the retina will be needed. This is usually done under a general anaesthetic and can be repaired with a single operation in 90 per cent of cases. This does not usually cause much pain but your eye will be sore and swollen for a few days afterwards. You will usually need to stay in the hospital for two or three days after your operation.
The two most common operations for retinal detachment are:-
- Scleral buckling – where a sponge or length of silicon plastic is placed on the outside of the eye and sewn in place, pushing the sclera (outer white tissue of the eye) toward the tear in the retina.
- Pneumatic retinopexy – a less severe treatment where the surgeon injects a gas bubble inside the vitreous cavity. The bubble pushes the retina against the wall of the eye, allowing the tear to seal itself against the eyewall.
Be aware that the eye surgeon (ophthalmologist) does not take your eye ‘out of its socket’ during the operation.
How much vision can I expect after a successful operation?
This depends on how much the retina has detached and for how long.
The shadow caused by the detachment will disappear in all cases when the retina has been put back in place. However, if the detachment involves the part of the retina that is responsible for your central vision, this may not recover. The longer this part of the retina has been detached, the smaller the chance that your central vision will recover to its former level. But, if this is the case, you will still have some useful vision left.
What happens after the operation?
Usually, you can return home after two or three days in the hospital. You will be encouraged to get up and carry on as usual on the day after the operation. Sometimes you will be asked to keep your head in a particular position to help the healing process.
You can resume normal activities as soon as you feel able. It might be week or two before you can drive a motor vehicle.
What happens if the retina is not put back in place?
Most people will lose all useful vision if no eye operation is carried out, or if the treatment is unsuccessful. Occasionally, if the detachment involves the lower portion of the retina, some vision may recover by itself.
Can retinal detachment be prevented?
If your family has a history of retinal detachment, or your optometrist or eye specialist finds a weakness in your retina then preventive laser or freezing treatment may be needed. In most cases, however, it is not possible to take preventive action.
Retinal detachment does not happen because of straining your eyes, bending or heavy lifting.
Am I likely to get one in the other eye?
If you have had a retinal detachment in one eye, you are at increased risk of developing one in the other eye. But, there is only about a one in ten chance of this happening.
What if my sight cannot be fully restored?
Much can be done to help you use your remaining vision as fully as possible. You should ask your optometrist or eye specialist to refer you to the hospital low vision clinic (LVA clinic). There are a variety of optical aids such as brighter reading lights, simple magnifying glasses and more sophisticated equipment that can help you.
Is there anything I can do to cope with these annoying floater symptoms?
Floaters can be particularly annoying. They get in the way of seeing things and can make some things difficult, for example reading a book. There is a way of trying to cope with this that some people find useful. If you move your eyes around you can create currents in the jelly within your eyes this can sometimes move the floater out of your direct field of vision. This works best if you have one large floater rather than lots of small ones. Making things bigger can also help while you have floaters so that you are able to see things around the blank spots the floaters cause. However, most people find that with time the floaters become less and less of a problem.
Will I need to visit my optometrist after seeing floaters or retinal detachment?
Yes, your optometrist will need to give you a thorough examination during your first visit. He will be able to pay special attention to whether or not the retina is still in any danger. If it isn’t then they may not need to see you again. However, if you begin to experience the symptoms warning of a possible retinal detachment, such as an increased or definite change in floaters more severe flashing lights and/or a ‘curtain’ or ‘veil’ falling over your vision then a trip to the optometrist will again be necessary.