What is age-related macular degeneration?
Age-related macula degeneration (ARMD or AMD) is when the delicate cells of the macula become damaged and stop working. We do not know why this is, although it tends to happen as people get older. Macular degeneration usually involves both eyes, although they may not be affected at the same time or to the same extent.
AMD is the leading cause of vision loss and blindness among the over 65 population in the UK. Because people in this group are an increasingly larger percentage of the general population, vision loss from macular degeneration is a rapidly growing problem.
Sometimes children and young people can also suffer from an inherited form of macular degeneration called macular dystrophy. Sometimes several members of a family will suffer from this, and if this is the case it is very important that you have your eyes checked at regular intervals.
What is the macula?
Imagine that your eye is like a camera. There is a lens and an aperture (the pupil) at the front, which both adjust to bring objects into focus on the retina at the back of your eye. The retina is made up of a delicate tissue that is sensitive to light, rather like the film in a camera.
The macula is found at the centre of the retina where the incoming rays of light are focused and is the part of the retina responsible for the sharp, central vision needed to read or drive. The macula is very important and is responsible for:
- what we see straight in front of us.
- the vision needed for detailed activities such as reading and writing.
- our ability to appreciate colours.
Wet and Dry forms of macular degeneration
Macular degeneration is diagnosed as either ‘dry’ (non-neovascular) or ‘wet’ (neovascular). The dry form is more common than the wet form, with about 85% to 90% of AMD patients diagnosed with dry AMD. The wet form of the disease usually leads to more serious vision loss.
Dry macular degeneration (non-vascular). Dry AMD is considered an early stage of the disease and may result from the ageing and thinning of macular tissues, depositing of pigment in the macula or a combination of the two processes.
Dry macular degeneration is diagnosed when yellowish spots known as drusen begin to accumulate in and around the macula. It is believed these spots are deposits or debris from deteriorating tissue.
Gradual central vision loss may occur with dry macular degeneration but usually, it is not nearly as severe as wet AMD symptoms. However, dry AMD through a period of years slowly can progress to late-stage geographic atrophy (GA) — gradual degradation of retinal cells that also can cause severe vision loss.
Wet macular degeneration (neovascular). In about 20% of cases of dry AMD, the disease progresses to the more advanced and damaging ‘wet’ form. In wet macular degeneration, new blood vessels grow beneath the retina and leak blood and fluid. This leakage causes permanent damage to light-sensitive retinal cells, which die off and create blind spots in the eye’s central vision.
Choroidal neovascularisation (CNV), the underlying process causing wet AMD and abnormal blood vessel growth, is the body’s misguided way of attempting to create a new network of blood vessels to supply more nutrients and oxygen to the eye’s retina. Instead, the process creates scarring, leading to sometimes severe central vision loss.
Wet macular degeneration falls into 2 categories:
- Occult. New blood vessel growth beneath the retina is not as pronounced, and leakage is less evident in the occult CNV form of wet macular degeneration, which typically produces less severe vision loss.
- Classic. When blood vessel growth and scarring have very clear, delineated outlines observed beneath the retina, this type of wet AMD is known as classic CNV, usually producing more severe vision loss.
- Occult. New blood vessel growth beneath the retina is not as pronounced, and leakage is less evident in the occult CNV form of wet macular degeneration, which typically produces less severe vision loss.
And now the good news
Macular degeneration is not painful and never leads to total blindness. It is the most common cause of poor sight in people over 60 years old but never leads to complete sight loss because it is only the central vision that is affected. Macular degeneration never affects vision at the outer edges of the eye. This means that almost everyone with macula degeneration will have enough side vision to get around and keep their independence.

In the early stages, your central vision may be blurred or distorted, with things looking an unusual size or shape. This may happen quickly or develop over several months. You may be very sensitive to light or actually see lights that are not there. Occasionally this may cause some visual discomfort. The macula enables you to see fine detail and people with the advanced condition will often notice a blank patch or dark spot in the centre of their sight. This makes activities like reading, writing and recognising small objects or faces very difficult.
Viewing a chart of black lines arranged in a graph pattern (Amsler grid) is one way to tell if you are having these vision problems. See how an Amsler grid works by taking a macular degeneration test.
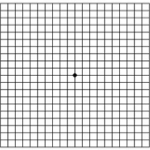
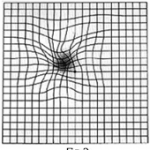
Other eye conditions such as an epiretinal membrane or cystoid macula oedema, central serous retinopathy can cause distortion in the centre of the Amsler charts so it cannot be always be assumed that distortion indicates AMD.
What should I do if I think I have age-related macular degeneration?
promptly who, if necessary, will refer you to an eye specialist. If macular degeneration has already been diagnosed in one of your eyes, and your other eye starts to get symptoms, then you should go to the hospital that usually looks after you, or your local casualty department, as soon as possible.
If you are suspected of having macular degeneration what does an examination involve?
Optometrists can detect the early signs of macular degeneration at your regular eye examination, often before symptoms occur. Usually, this is accomplished through a retinal exam or 3D OCT eye scan.
Firstly there will be an assessment of your vision in both eyes. You may be given eye drops which enlarge your pupil so that your eye specialist or optometrist can look into your eyes. The drops take about 20 minutes to work although their effect may last for several hours. Your vision will become blurred for a while and your eyes will become very sensitive to light, but this is nothing to worry about. It is always a good idea to bring a pair of sunglasses to the examination for use afterwards. You will not be able to see well enough to drive yourself home after your examination, ask a friend or relation to drive you to the clinic. When macular degeneration is suspected, a brief test using the Amsler grid that measures your central vision may be performed.
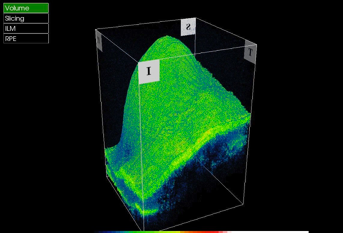
Your specialist may look into your eyes with a number of different instruments. These may include an ophthalmoscope, a tonometer and a slit-lamp microscope. It may be that your specialist requests further investigations to be done. This might involve a 3D OCT eye scan and fluorescein angiography. Both of these tests allow your eye specialist or optometrist to tell the type (wet or dry) and amount of AMD you have and will help decide on the best type of treatment for you.
What is 3D OCT?
Optical Coherence Tomography is fast becoming the diagnostic method of choice in busy NHS macular degeneration clinics due to its quick, non-invasive and entirely painless process. For further details see 3D OCT eye scan.
What is fluorescein angiography?
In some cases, your eye specialist may decide that a fluorescein angiogram will be needed. You will visit your local hospital eye clinic for this examination. These photographs give an accurate map of the changes occurring in the blood circulation of the macula and help your eye specialist to decide what is the best treatment for you. For the angiogram, you will be given a small injection of special dye in your arm which then works its way around the circulation of your eyes. This is not painful but you may feel a bit sick afterwards. A series of rapid pictures of your retina are then taken with blue light over the next few minutes. There are few side effects, although some people find that they are dazzled for a while afterwards. You may also notice that the injection has left your skin with a faint yellow tinge from the fluorescein dye but this soon passes as it is excreted in your urine.
Who gets age-related macular degeneration?
Besides affecting older populations, AMD occurs in Caucasians and females in particular. The disease also can result as a side effect of some drugs, and it seems to run in families.
New evidence strongly suggests smoking is high on the list of risk factors for macular degeneration. Other risk factors for macular degeneration include having a family member with AMD, high blood pressure, lighter eye colour and obesity.
Some researchers believe that over-exposure to sunlight also may be a contributing factor in the development of macular degeneration, but this theory has not been proven conclusively. High levels of dietary fat also may be a risk factor for developing AMD.
The only risk factors consistently found in studies to be associated with eye disease are ageing and smoking.
Commonly named risk factors for developing macular degeneration include:
- Ageing. Significant vision loss accompanying more advanced forms of AMD increases from fewer than 1 per cent among people in their 60s to more than 15 per cent among people in their 90s, according to the Canadian Medical Association Journal (February 2004).
- Smoking. Smoking is a major AMD risk factor and was found in one British study to be directly associated with about 25 per cent of AMD cases causing severe vision loss. The British Journal of Ophthalmology in early 2006 also reported study findings showing that people living with a smoker double their risk of developing AMD.
- Obesity & Inactivity. Overweight patients with macular degeneration had more than double the risk of developing advanced forms of macular degeneration compared with people of normal body weight, according to one study reported in Archives of Ophthalmology (June 2003). In the same study, those who performed vigorous activity at least three times weekly reduced their risk of developing advanced AMD, compared with inactive patients
- Heredity. As stated above, recent studies have found that specific variants of different genes are present in most people who have macular degeneration. Studies of fraternal and identical twins may also demonstrate that heredity is a factor in who develops AMD and how severe it becomes.
- High Blood Pressure (Hypertension). Investigative Ophthalmology and Vision Science reported the results of a European study demonstrating that high blood pressure may be associated with the development of macular degeneration (September 2003).
- Lighter Eye Colour. Because macular degeneration long has been thought to occur more often among Caucasian populations, particularly in people with light skin colour and eye colour, some researchers theorised that the extra pigment found in darker eyes was a protective factor against the development of the eye disease during sun exposure. But no conclusive evidence as yet has linked excessive sun exposure to development of AMD.
- Drug Side Effects. Some cases of macular degeneration can be induced from side effects of toxic drugs such as chloroquine (an anti-malarial drug) or phenothiazine. Phenothiazine is a class of antipsychotic drugs, including brand names of Thorazine (chlorpromazine, which also is used to treat nausea, vomiting and persistent hiccups), Mellaril (thioridazine), Prolixin (fluphenazine), Trilafon (perphenazine), Stelazine (trifluoperazine) and Stemitil (prochlorperazine).
- Ageing. Significant vision loss accompanying more advanced forms of AMD increases from fewer than 1 per cent among people in their 60s to more than 15 per cent among people in their 90s, according to the Canadian Medical Association Journal (February 2004).
How is macular degeneration treated?
There is as yet no outright cure for age-related macular degeneration, but some treatments may delay its progression or even improve vision.
Treatments for macular degeneration depend on whether the disease is in its early-stage, dry form or in the more advanced wet form that can lead to serious vision loss. No NICE–approved treatments exist yet for dry macular degeneration, although nutritional intervention may help prevent its progression to the wet form.
For wet AMD, treatments aimed at stopping abnormal blood vessel growth include the NICE–approved drug Lucentis. Lucentis has been shown to improve vision in a significant number of people with macular degeneration.
Neovascularization is activated by a protein called vascular endothelial growth factor (VEGF), these are targeted in macular degeneration treatments by anti-VEGF drugs such as Lucentis ® and Avastin ®
Nutrition and dry macular degeneration
Many researchers and eye care practitioners believe that certain nutrients — zinc, lutein, zeaxanthin and vitamins A, C and E — help lower the risk for AMD or slow down the progression of dry macular degeneration. Benefits of high levels of antioxidants and zinc for halting or slowing the development of AMD have been widely reported based on results released in 2001 from the Age-Related Eye Disease Study (AREDS) conducted by the National Eye Institute in the USA.
A number of proprietary products such as Macushield ®, ICaps ® and Ocuvite ® may reduce risk of early-stage AMD progression by 25 per cent. We stock all of these products at Paul Whiteman Optometrists.
Optometrists and ophthalmologists also recommend that dry AMD patients wear UV blocking sunglasses to protect against the potentially harmful effects of the sun.
Testing and low vision devices for macular degeneration treatment
Although much progress has been made recently in macular degeneration treatment research, complete recovery of vision lost to AMD is unlikely.
Your optometrist may ask you to check your vision regularly with the Amsler grid described above.
Viewing the Amsler grid separately with each eye helps you monitor your vision loss. The Amsler grid is a very sensitive test and it may reveal central vision problems before your optometrist sees AMD-related damage to the macula in a routine eye examination
For those who have vision loss from macular degeneration, many low vision & magnifier devices are available to help with mobility and specific visual tasks.
What research is going on?
There is a great deal of research that is looking into the causes of macular degeneration and how it can be treated. With ‘dry’ degeneration there have been claims that certain types of medical therapy can halt the condition, but this currently remains uncertain.
You can find out more from the:
Macular Disease Society
PO Box 247
Haywards Heath
West Sussex
RH17 5FF
HELPLINE: 0845 241 2041
Telephone 0990 143 573
For further information about RNIB services please contact them at:
Royal National Institute for the Blind
105 Judd Street
London
WC1H 9NE
Telephone 0345 766 9999
For help with living and coping with AMD contact:
Rentwood
School Lane
Fetcham
Leatherhead
Surrey
KT22 9JX
Telephone 01372 377 701